Bilateral Salpingo Oophorectomy Surgery: A Comprehensive Guide
Understanding Bilateral Salpingo Oophorectomy Surgery
The term bilateral salpingo oophorectomy surgery refers to a surgical procedure in which both ovaries and fallopian tubes are surgically removed. This procedure is often performed in cases of ovarian cancer, severe endometriosis, or other significant gynecological conditions. Understanding this surgery is vital for patients considering this procedure, as it has profound implications for their health and fertility.
Why Is Bilateral Salpingo Oophorectomy Done?
There are several medical reasons why a healthcare professional might recommend a bilateral salpingo oophorectomy, including:
- Ovarian Cancer: This surgery is a common treatment option for women diagnosed with ovarian cancer.
- Severe Endometriosis: Women suffering from severe endometriosis may find relief through this procedure.
- Genetic Predisposition: Women with BRCA gene mutations may opt for this surgery as a preventive measure against breast and ovarian cancer.
- Adnexal Masses: If cysts or masses on the ovaries are symptomatic or suspicious, surgical removal might be necessary.
- Persistent Ovarian Pain: If other treatments fail, this surgery can alleviate chronic pain.
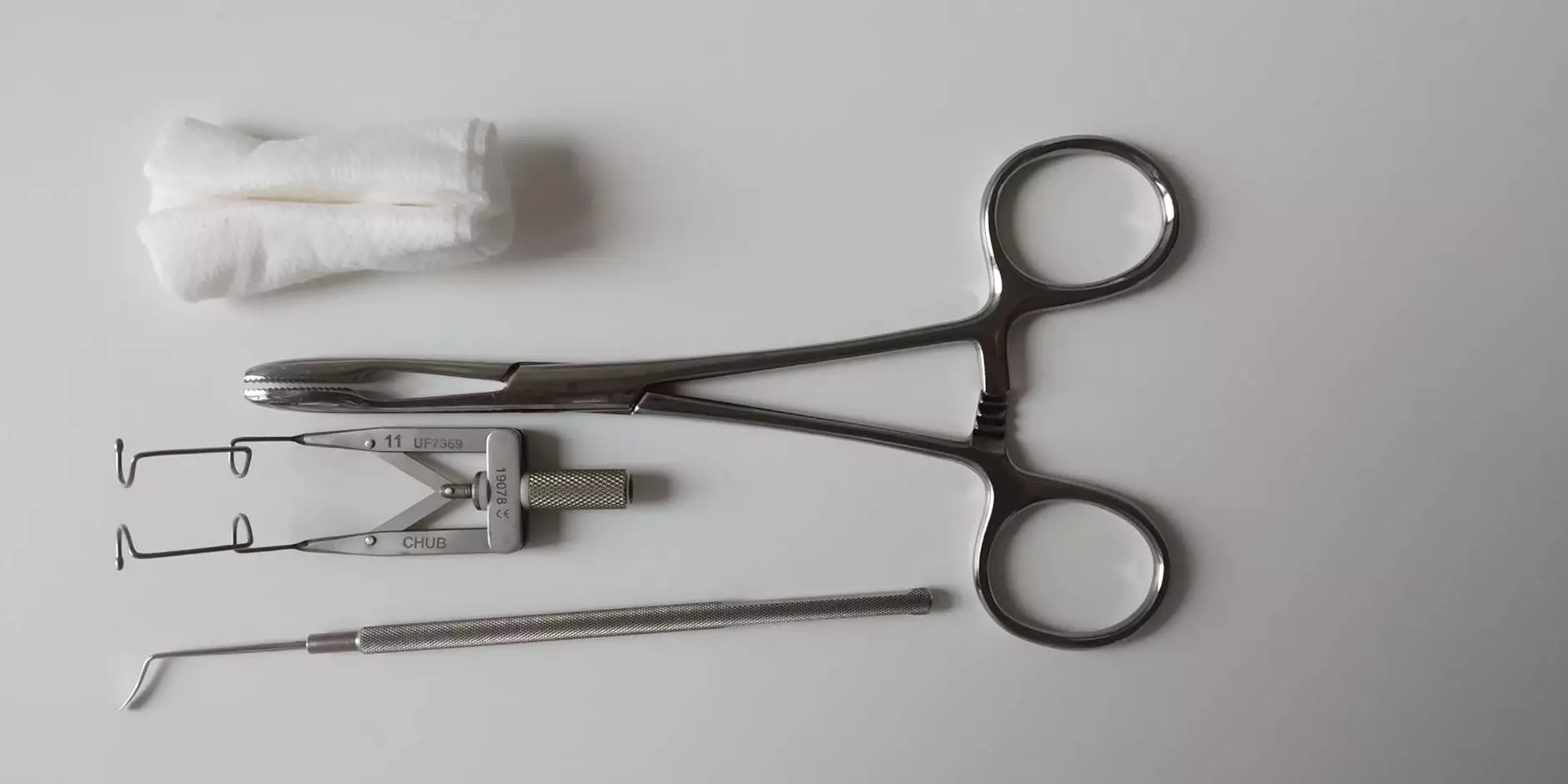
The Surgical Procedure: What to Expect
The bilateral salpingo oophorectomy surgery is typically performed under general anesthesia. The specific surgical approach varies based on the individual patient’s circumstances and the surgeon’s recommendations:
Laparoscopic Approach
This minimally invasive technique involves small incisions in the abdomen through which a camera and specialized surgical instruments are inserted. The benefits of laparoscopy include:
- Reduced recovery time
- Less postoperative pain
- Smaller scars
Open Surgery
In some cases, an open surgical approach may be necessary. This involves a larger abdominal incision and may be chosen if the condition is complicated or when larger masses need to be removed.
Preoperative Considerations
Before undergoing surgery, a thorough preoperative assessment is crucial. This might include:
- Physical Examination: A complete evaluation to determine the patient’s health status.
- Imaging Tests: Ultrasounds or CT scans to understand the condition of the ovaries and tubes.
- Blood Tests: To check hormone levels and other health indicators.
- Consultation: Discussion of potential risks and complications of the surgery.
Risks and Complications of Bilateral Salpingo Oophorectomy
Like any surgical procedure, bilateral salpingo oophorectomy surgery carries risks, which may include:
- Infection: Risk of infection at the surgical site.
- Bleeding: Potential for significant blood loss during or after surgery.
- Hormonal Changes: Removal of the ovaries leads to hormonal changes, potentially causing menopause if the patient is pre-menopausal.
- Damage to Surrounding Organs: Unintentional injury to nearby organs such as the bladder or intestines.
- Chronic Pain: Some women may experience ongoing pelvic discomfort following the surgery.
The Recovery Process
The recovery period can vary based on the surgical approach:
Laparoscopic Recovery
Patients can often return home within a few hours post-surgery and may resume normal activities within a few days to weeks.
Open Surgery Recovery
In contrast, recovery from open surgery might take several weeks, during which patients should avoid heavy lifting and strenuous activities.
Postoperative Care and Follow-Up
After the surgery, follow-up appointments are essential to monitor recovery. Key components of postoperative care include:
- Pain Management: Managing pain with prescribed medications.
- Activity Modification: Following guidelines on physical activity to prevent complications.
- Hormone Therapy: Discussing hormone replacement therapy if necessary.
- Emotional Support: Acknowledging the emotional and psychological impacts of the surgery.
Long-Term Health Implications
Women who undergo bilateral salpingo oophorectomy surgery should be aware of the long-term health implications:
- Menopause: If the surgery is performed before natural menopause, patients may enter menopause immediately.
- Infertility: Removal of the ovaries and fallopian tubes results in infertility.
- Increased Risk of Cardiovascular Disease: The absence of ovarian hormones can increase cardiovascular risks.
- Bone Health: There is a potential increase in osteoporosis due to hormonal changes.
Why Choose Experienced Healthcare Professionals
Choosing a knowledgeable and experienced healthcare provider, such as those at Dr. Seckin's practice, is paramount for women considering this surgery. An expert can provide:
- Comprehensive Assessments: Detailed evaluations to understand the patient's unique health profile.
- Personalized Treatment Plans: Tailored approaches to surgery and recovery based on individual needs.
- Emotional Support: Guidance and counseling during the emotional journey post-surgery.
- Access to Resources: Referrals to support groups and educational materials.
Conclusion: Empowering Your Health Choices
Bilateral salpingo oophorectomy surgery can be a significant step in managing serious gynecological conditions. Understanding the procedure, its risks, and its implications for health and fertility is essential for empowering women to make informed decisions. By consulting experienced medical professionals, patients can navigate this challenging time with confidence and support.
If you or a loved one are considering bilateral salpingo oophorectomy surgery, it’s important to seek advice from a healthcare provider who specializes in gynecological surgery. For more information about this procedure and expert care, visit Dr. Seckin's website today.



